Quick Links
Uvea
The uvea is the middle layer of the eye, situated between the sclera (white outer coat) and the retina (light-sensitive inner layer). It comprises three key structures — the iris (colored part of the eye), ciliary body (controls lens shape and fluid production), and choroid (nourishes the retina). The uvea plays a critical role in eye function, contributing to light regulation, nutrient transport, and intraocular pressure maintenance.
Inflammation of the uveal tract is known as uveitis, a condition that can range from mild and short-lived to severe and vision-threatening. Uveitis can affect one or both eyes, occur at any age, and may involve any part of the uvea. Early diagnosis and precise treatment are crucial to prevent permanent visual impairment.
Read More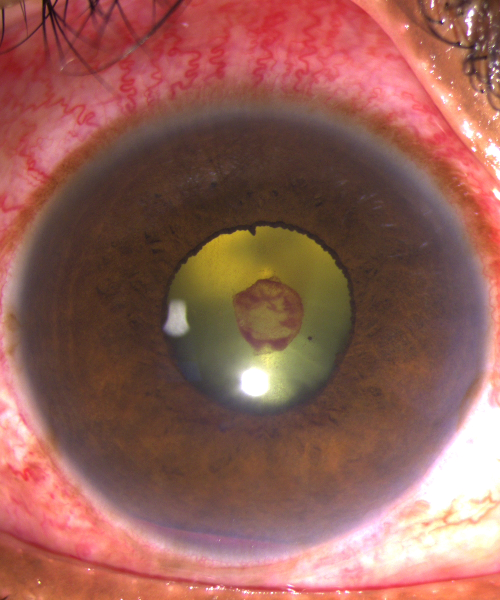
Types of Uveitis
Uveitis is classified based on the part of the uvea that is inflamed:
Anterior Uveitis
The most common type, affecting the iris and anterior chamber. It presents with redness, pain, photophobia, and blurred vision. Often linked to autoimmune diseases, but can also be idiopathic.
Intermediate Uveitis
Involves inflammation in the vitreous and peripheral retina. Symptoms include floaters and blurred vision, usually without redness or pain. Common in young adults and may be associated with systemic diseases like sarcoidosis or multiple sclerosis.
Posterior Uveitis
Affects the retina and choroid, causing decreased vision, floaters, or visual field defects. It often results from infections like toxoplasmosis or autoimmune conditions such as Behçet’s disease.
Panuveitis
Involves all layers of the uveal tract and often presents with widespread inflammation, pain, and significant vision loss. This is the most severe form and typically requires aggressive management.
Symptoms of Uveitis
Eye Redness and Pain
Often one of the earliest and most noticeable signs, caused by inflammation in the anterior portion of the eye. The pain may range from mild irritation to deep, throbbing discomfort.
Blurred or Decreased Vision
Inflammation can affect the clarity of vision, either through swelling, fluid accumulation, or involvement of the retina and vitreous. This may worsen over time without treatment.
Photophobia (Light Sensitivity)
Inflamed eyes are more sensitive to light, leading to discomfort even in normal lighting. This is particularly common in anterior uveitis.
Floaters or Dark Spots in Vision
Patients may notice moving spots, cobweb-like shadows, or specks due to inflammatory cells in the vitreous cavity. This is frequently seen in intermediate and posterior uveitis.
Tearing or Excessive Watering
The eye may produce more tears in response to inflammation, though this is not always a sign of infection.
Headache or Aching Around the Eyes
Inflammation may radiate discomfort to surrounding areas, especially if the ciliary body or optic nerve is involved.
Visual Field Defects
In advanced or posterior uveitis, damage to the retina can lead to peripheral vision loss, blind spots, or difficulty seeing in certain directions.
Causes of Uveitis
Autoimmune Disorders
Conditions such as rheumatoid arthritis, lupus, ankylosing spondylitis, or sarcoidosis can trigger the immune system to attack the uveal tract of the eye, leading to chronic or recurrent inflammation without any direct infection.
Infections
Certain viral, bacterial, or parasitic infections can cause uveitis. Common culprits include tuberculosis, herpes simplex or zoster, syphilis, and toxoplasmosis. These may affect different layers of the eye depending on the organism involved.
Systemic Inflammatory Diseases
Disorders like Crohn’s disease, ulcerative colitis, and multiple sclerosis may cause immune-mediated inflammation that involves the eye, especially in intermediate or posterior uveitis.
Ocular Trauma or Surgery
Injury to the eye or recent intraocular procedures can result in an inflammatory response. This may manifest as post-traumatic uveitis or post-operative inflammation requiring close monitoring.
Idiopathic Causes
In many patients, no specific cause is found even after extensive testing. These cases are termed idiopathic uveitis and still require appropriate treatment and regular follow-up to prevent complications.
Uveitis Treatment Options
Treatment is tailored based on the cause, type, and severity of the uveitis:
Topical Medications
Steroid Eye Drops
Reduce inflammation in anterior uveitis
Mydriatic Drops
Help relieve pain and prevent synechiae (adhesions)
Systemic Therapy
Oral Steroids
For posterior or panuveitis or when topical therapy is insufficient.
Immunosuppressants
Such as methotrexate, azathioprine, or biologics like adalimumab in chronic or autoimmune-related uveitis.
Antibiotics/Antivirals
In infectious causes like toxoplasmosis or herpetic uveitis.
Periocular or Intraocular Injections
Steroid Injections
Directly deliver medication to inflamed areas when systemic side effects must be minimized.
Surgical Management
Vitrectomy
For persistent vitreous opacities or complications such as retinal detachment or diagnostic biopsy.
Cataract Surgery
May be needed if long-standing inflammation or steroid use causes lens opacity
Complications of Uveitis
Chronic inflammation or prolonged steroid treatment can cloud the natural lens of the eye, leading to vision loss that may require surgical correction.
Cataract Formation
Chronic inflammation or prolonged steroid treatment can cloud the natural lens of the eye, leading to vision loss that may require surgical correction.
Glaucoma
Inflammation or steroid use can increase intraocular pressure, damaging the optic nerve over time and resulting in progressive vision loss.
Macular Edema
Swelling in the central retina (macula) can blur central vision, affecting tasks like reading and recognizing faces.
Retinal Detachment
Severe inflammation may cause structural damage, increasing the risk of the retina pulling away from its underlying tissue—a vision-threatening emergency.
Optic Nerve Damage
Persistent inflammation near the optic nerve can impair its function, leading to permanent blind spots or decreased visual clarity.
Permanent Vision Loss
Without proper and timely treatment, uveitis can damage essential structures of the eye, resulting in irreversible loss of sight.
FAQ's
What is uveitis?
Uveitis is inflammation of the uveal tract of the eye, which includes the iris, ciliary body, and choroid. It can also affect adjacent structures like the retina and vitreous, leading to vision problems if not treated early.
What causes uveitis?
Uveitis can be caused by autoimmune conditions, infections, trauma, or systemic inflammatory diseases. In many cases, the exact cause may remain unknown (idiopathic).
Is uveitis a serious condition?
Yes, if left untreated, uveitis can lead to complications like glaucoma, cataract, retinal damage, and permanent vision loss. Early diagnosis and treatment are essential.
What are the symptoms of uveitis?
Common symptoms include eye redness, pain, blurred vision, light sensitivity, floaters, and occasionally headache or visual field loss.
How is uveitis diagnosed?
A detailed eye examination, including slit-lamp evaluation, fundus examination, and imaging like OCT or fluorescein angiography, helps confirm the diagnosis. Blood tests and scans may also be done to identify underlying causes.
