Laser Procedures for Glaucoma
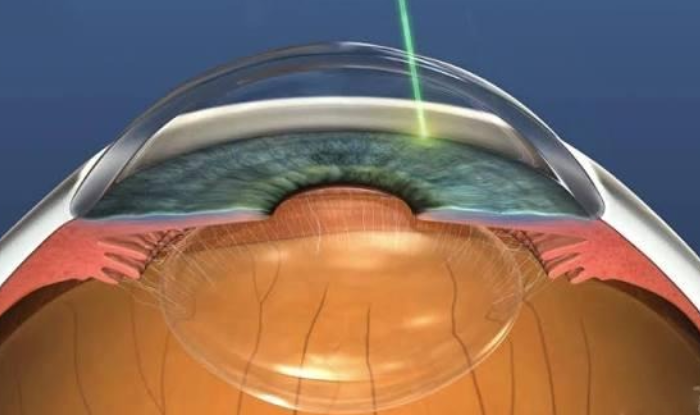
Laser treatments for glaucoma use a focused beam of light to lower intraocular pressure (IOP), which helps prevent or slow damage to the optic nerve. These outpatient procedures can improve the eye's natural fluid drainage or reduce fluid production. The specific laser procedure recommended depends on the type and severity of glaucoma
Types of Laser Procedures
Selective Laser Trabeculoplasty (SLT)
This is a common treatment for open-angle glaucoma, where the eye's drainage angle is open but inefficient
Mechanism
A low-energy laser is used to treat specific pigmented cells in the trabecular meshwork (the eye's drainage tissue). This triggers a biological change that improves fluid outflow.
Benefits
Because it uses a low-level, non-destructive laser, SLT can be repeated if the pressure-lowering effect wears off over time.
Efficacy
Studies show that SLT is as effective as eye drops in lowering IOP and is often a preferred first-line treatment option.
Closing
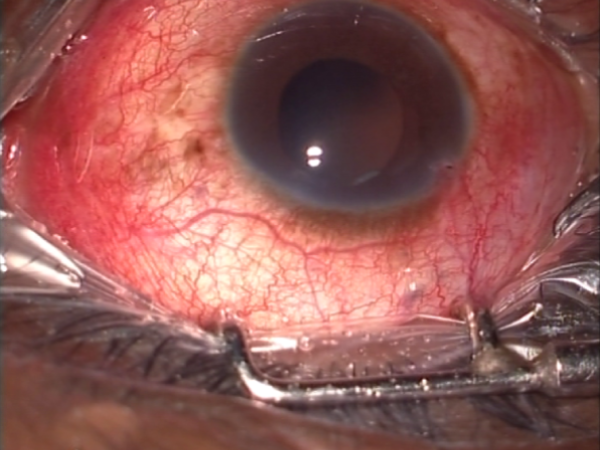
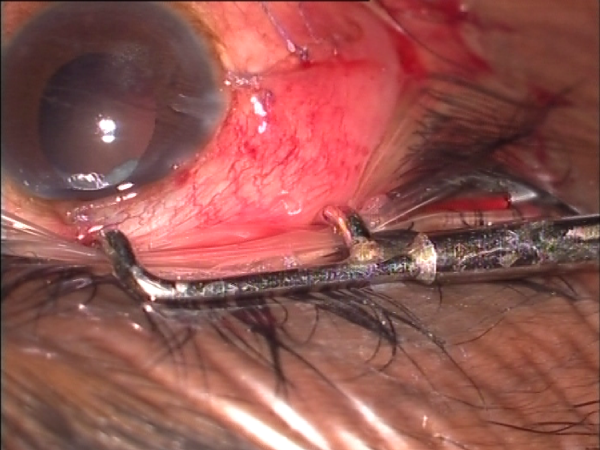
Dissolving sutures are used to repair the incision in the conjunctiva.
Laser Peripheral Iridotomy (LPI)
LPI is primarily used for angle-closure glaucoma, where the iris blocks the eye's drainage angle.
Mechanism
The laser creates a small hole in the outer edge of the iris, creating an alternative pathway for fluid to flow more freely.
Benefits
It can quickly relieve the dangerously high pressure associated with an acute angle-closure attack. It is also used as a preventative measure for people with narrow angles.
Cyclophotocoagulation (CPC)
This procedure is typically reserved for advanced or refractory glaucoma cases where other treatments have been ineffective.
Mechanism
The laser targets the ciliary body, the part of the eye that produces the aqueous fluid. This reduces fluid production, thereby lowering IOP.
Types
Transscleral CPC (TSCPC) applies the laser externally through the sclera, while endoscopic CPC (ECP) uses a tiny camera inside the eye to guide the laser more precisely.
Glaucoma Surgeries
Glaucoma surgery lowers intraocular pressure (IOP) to prevent further optic nerve damage and vision loss. Procedures include trabeculectomy, which creates new drainage channels in the eye, glaucoma drainage implants (tube shunts), which involve a small tube draining fluid to a plate under the eyelid, and Minimally Invasive Glaucoma Surgery (MIGS), which uses tiny implants or stents to improve the eye's natural drainage system.
The choice of surgery depends on the individual's glaucoma severity and response to other treatments.
Types of Glaucoma Surgery
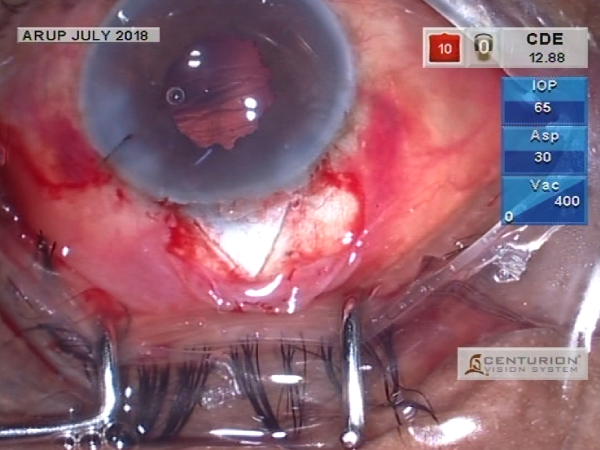
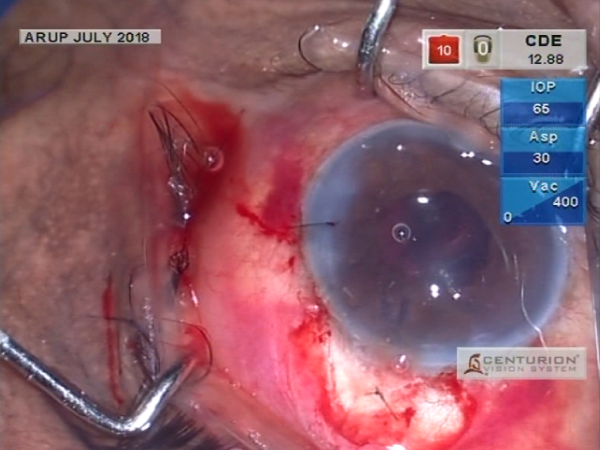
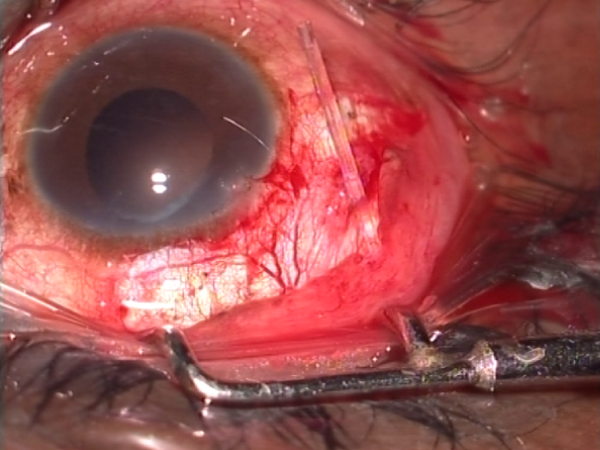
Trabeculectomy
A more invasive procedure where the surgeon creates a small flap in the white part of the eye and a new pathway for fluid to drain. This fluid collects in a small blister (bleb) under the upper eyelid and is absorbed into the bloodstream.
Glaucoma Drainage Implants (Tube Shunts)
A small, plastic tube with a plate is surgically inserted to drain fluid from the eye into a collection area under the eyelid.
Minimally Invasive Glaucoma Surgery (MIGS)
A category of less invasive procedures that use tiny implants or devices to enhance the eye's natural drainage system.
Purpose
Glaucoma surgery aims to lower eye pressure and prevent further vision loss; it cannot restore vision already lost.
Procedure Duration
Laser procedures are very quick, while MIGS and traditional surgeries can take longer, especially if combined with phacoemulsification and IOL implantation to manage the associated cataract
Recovery
Postoperative care is crucial and requires attention to immediate and long-term care to prevent complications.
Combined Procedures
Glaucoma surgery is often combined with cataract surgery to address both conditions at once.
Advantages and Considerations
Advantages
Minimally Invasive
Most procedures are performed in a doctor's office in minutes, with a faster recovery time than traditional surgery.
Fewer Medications
Laser treatment can reduce or eliminate the need for daily eye drops for many patients.
Effective Results
For many, the treatment effectively lowers eye pressure and slows the progression of the disease.
Potential side effects and risks
Transient IOP spike
A temporary increase in eye pressure is possible immediately after the procedure.
Inflammation
Some patients may experience mild inflammation, which can cause redness, discomfort, and light sensitivity.
Blurry Vision
Temporary blurry vision is common for a few hours after the procedure.
Ineffective or Temporary Results
In some cases, the treatment may not be successful or the effects may wear off over time, requiring additional procedures or medications.
How to decide
If you have glaucoma, your ophthalmologist will determine the best course of action for your specific condition. The decision will factor in the type of glaucoma, severity, and overall eye health. For some, laser therapy may be the first treatment, while for others it may be a supplemental or later-stage treatment.
Choosing the Right Procedure
- The best type of surgery depends on the individual's condition, the severity of glaucoma, and their response to previous treatments.
- More invasive procedures like trabeculectomy and tube shunts are often used for severe or complex glaucoma when other treatments have failed